Alcohol consumption has long been associated with the risk of liver damage, including conditions such as alcoholic fatty liver disease, alcoholic hepatitis, and cirrhosis. This article will explore the intricacies of liver health and alcohol research, the impact of excessive alcohol intake, and the potential for liver recovery.
Types of Alcohol-Related Liver Diseases
Alcoholic Fatty Liver Disease (AFLD):
Alcoholic Hepatitis:
Alcoholic Cirrhosis:
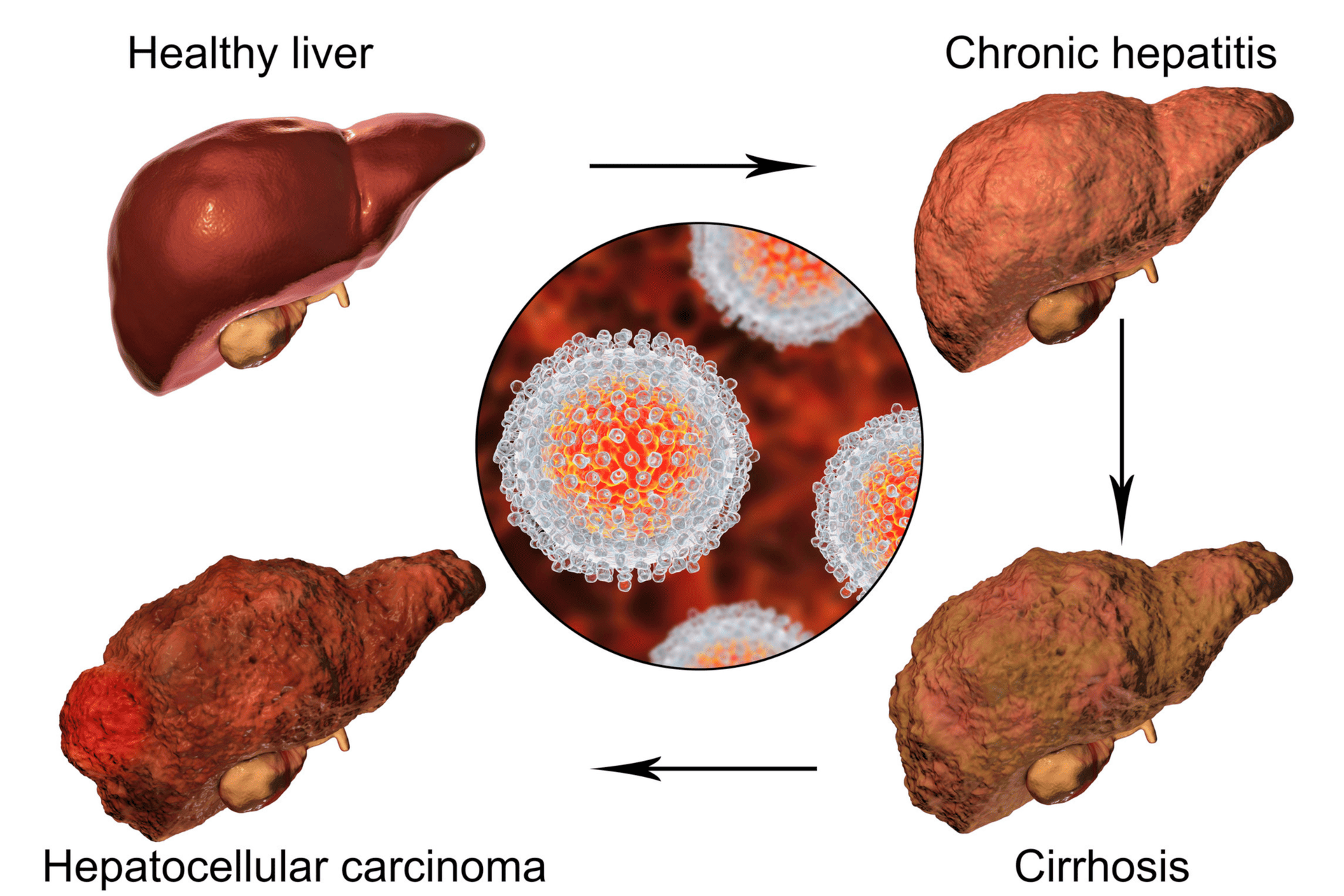
Cirrhosis is the advanced stage of alcoholic liver disease. It involves the development of scar tissue in the liver, which can lead to liver failure. Cirrhosis is often irreversible, making it crucial to address liver disease early on.
Can a Liver Heal From an Alcohol-Related Liver Disease?
The liver’s ability to recover from excess alcohol intake and-induced damage depends on various factors. Early intervention and severity of damage are some of the key factors in the liver’s ability to heal. Mild Alcoholic Hepatitis in its initial stages, alcoholic hepatitis can be reversible if alcohol use is stopped promptly. The liver can then initiate the healing process.
Unfortunately, in advanced stages of alcohol-related liver diseases like cirrhosis, the damage may be irreversible. The liver’s capacity to repair itself is limited, and this can result in end-stage liver disease, often necessitating a liver transplant.
Alcoholic Liver Disease Complications
Alcohol affects the liver in several ways, leading to various forms of damage. It’s essential to understand the processes involved in this damage to appreciate the potential for recovery.
Metabolizing Alcohol: The liver plays a central role in metabolizing alcohol. It breaks down alcohol into substances that can be eliminated from the body. However, this process can generate harmful byproducts, leading to oxidative stress and inflammation.
Fatty Liver Disease: Excessive alcohol intake can lead to the accumulation of fat in liver cells. This condition, alcoholic fatty liver disease, is often reversible by quitting alcohol and lifestyle changes.
Inflammation: Chronic alcohol use can lead to inflammation in the liver, which is a hallmark of alcoholic hepatitis. While mild cases may recover by quitting drinking alcohol, severe cases can progress to cirrhosis.
Scar Tissue Development: As inflammation persists, the liver attempts to repair itself by forming scar tissue. This can lead to cirrhosis, a stage where the liver’s regenerative capacity is significantly impaired.
Cirrhosis Progression
Cirrhosis, the end-stage of alcoholic liver disease, is characterized by extensive scarring in the liver. The progression of liver cirrhosis often involves several key factors:
Continued Excessive Drinking: Cirrhosis typically worsens if alcohol use continues. As the liver’s ability to regenerate diminishes, the damage becomes irreversible.
Complications and Death Rates: Cirrhosis is associated with various complications, including portal hypertension, spontaneous bacterial peritonitis, and acute pancreatitis. These complications can lead to significant health risks and increased death rates.
Blood Vessels and Blood Aiding Digestion
The liver is a vital organ for digestion, as it processes the nutrients absorbed from the intestines. Blood vessels play a significant role in this process, ensuring that the liver can perform its functions effectively.
Blood Supply to the Liver: The liver receives a substantial amount of blood to aid in digestion. This blood carries nutrients from the intestines and plays a central role in the metabolic functions of the liver.
Portal Hypertension: Cirrhosis can lead to portal hypertension, a condition where blood flow is obstructed. This can result in complications such as esophageal varices and ascites.
The Importance of Early Intervention
The key to liver recovery from alcohol-related damage is early intervention. Detecting alcohol-related liver disease or issues in their initial stages and taking action can significantly improve the chances of recovery.

Mild Alcoholic Hepatitis (MAH)
In cases of MAH, where liver damage is in its early stages, intervention can lead to significant recovery. Individuals experiencing mild to severe alcoholic hepatitis may exhibit symptoms such as jaundice, abdominal discomfort, and a general feeling of unwellness.
Jaundice: Yellowing of the skin and eyes is a common symptom of liver dysfunction. It is often associated with MAH and can be reversible with prompt intervention.
Abdominal Pain: Pain or discomfort in the upper right abdomen is another symptom that can indicate liver issues. Addressing this pain and its underlying cause is essential for recovery.
Drowsiness and Vomiting Blood: In severe cases of alcoholic hepatitis, symptoms can progress to drowsiness and even vomiting blood. These are signs of advanced liver damage and should prompt immediate medical attention.
Lifestyle Changes and Their Impact on Liver Recovery

Healthy Diet and Liver Disease
Diet plays a crucial role in liver recovery. A well-balanced, nutritious diet can support the healing process and improve overall health. Here’s how dietary choices can aid in liver recovery:
Nutrient-Rich Diet: A diet rich in essential nutrients, including vitamins, minerals, and antioxidants, can help repair damaged liver cells. Foods like fruits, vegetables, whole grains, lean protein, and healthy fats should be prioritized.
Low-Fat Diet: Excessive fat in the diet can exacerbate liver issues, especially in cases of fatty liver disease. A low-fat diet is often recommended to reduce the burden on the liver.
Blood Sugar Regulation: Keeping blood sugar levels stable is vital, as fluctuations can contribute to liver damage. Focus on consuming complex carbohydrates and avoiding excessive sugar intake.
Digestive Enzymes: Certain foods and supplements can aid in the digestion and absorption of nutrients, reducing the workload on the liver.
Blood Pressure (BP) Control
High BP, or hypertension, can significantly affect the liver. It can lead to complications and worsen existing liver damage. Controlling BP is essential for promoting liver recovery.
Blood Pressure Medications: Individuals with high BP may require medications to control their condition. These medications can help reduce the strain on the liver.
Lifestyle Changes: Adopting a heart-healthy lifestyle that includes a balanced diet, regular exercise, and stress management can contribute to better control.
Quitting Drinking Alcohol
Immediate Alcohol Cessation: Stopping drinking alcohol immediately is the first and most critical step in preventing further liver damage and giving the liver a chance to heal.
Alcohol Addiction Support: Overcoming alcohol addiction can be challenging. Seek support from healthcare professionals or support groups specializing in addiction recovery.
Liver Function Test
Regular monitoring through liver function tests is crucial for assessing progress. These tests help track improvements in the liver and guide the treatment plan. They also provide valuable insights into how the liver responds to intervention.
Continued Monitoring: It’s essential to continue monitoring liver function, even after initial improvements are observed. This ongoing assessment ensures that the liver continues to heal and recover.
Individualized Treatment: Healthcare professionals can tailor treatment plans to meet the unique needs of each patient. This may include dietary recommendations, medication, and counseling.
Alcohol Addiction Support

Overcoming alcohol addiction can be challenging, and it often requires comprehensive support. There are various resources and strategies available to help individuals on their journey to recovery:
Support Groups: Joining support groups or attending Alcoholics Anonymous (AA) meetings can provide a sense of community and shared experiences. These groups offer a safe space to discuss challenges and successes.
Counseling and Therapy: Professional counseling or therapy can help individuals address the underlying causes of their alcohol addiction and develop coping strategies.
Medications: In some cases, healthcare providers may prescribe medications to help individuals manage alcohol cravings and reduce the risk of relapse.
Inpatient Rehabilitation: For severe cases of alcohol addiction, inpatient rehabilitation programs may be necessary. These programs provide intensive support and treatment in a structured environment.
Alcohol and the Liver: What You Need to Know
Chronic Binge Drinking and Alcohol Use
Chronic and excessive alcohol use is a leading cause of liver damage. Understanding alcohol-associated liver disease and how excessive alcohol use affects the liver is essential for anyone concerned about their liver health.
Oxidative Stress: The breakdown of alcohol in the liver produces harmful byproducts that can cause oxidative stress. This stress leads to inflammation and cell damage.
Alcohol-Induced Liver Disease: Excessive alcohol consumption can lead to a spectrum of liver diseases, from fatty liver to alcoholic cirrhosis to. The risk of developing these conditions is directly linked to the quantity and duration of alcohol use.
Liver Filters Alcohol: The liver is responsible for processing and filtering alcohol from the bloodstream. However, this continuous exposure to alcohol can lead to damage over time.
Kidney Failure and Alcohol-Related Liver Damage
The impact of alcohol abuse extends beyond the liver, affecting other vital organs such as the kidneys.
Kidney Function: The kidneys play a crucial role in filtering waste products and maintaining fluid and electrolyte balance in the body. Chronic alcohol use can disrupt kidney function, leading to failure.
Associated Kidney Failure: The development of alcoholic cirrhosis and related complications can contribute to failure. This complex relationship underscores the importance of early intervention and treatment.
Blood and Liver Disease
Blood plays a vital role in supporting liver functions and overall health. Understanding how blood and the liver are interconnected is crucial for those seeking to recover from alcohol-related liver damage.
Blood Aiding Digestion: Blood carries nutrients absorbed from the intestines to the liver, where they are processed and distributed throughout the body. This process is essential for digestion and overall health.
Blood Vessels and Liver Function: Blood vessels ensure that the liver receives the necessary nutrients for its metabolic functions. Healthy blood flow is essential for optimal liver function.
Circulatory Complications: In cases of advanced liver damage, circulatory complications can arise. These complications can have widespread effects on the body and further emphasize the importance of early intervention.
Overcoming Alcohol Addiction

Alcohol Addiction: The First Step Toward Recovery
Recognizing and addressing alcohol addiction is a critical component of liver recovery. Here’s what you need to know about overcoming alcohol addiction:
End-Stage Liver Disease: For individuals in the advanced stages of alcohol-induced liver disease, such as cirrhosis, addressing alcohol misuse and addiction becomes a matter of life and death.
Increased Risk: The risk of complications and death rates is significantly higher for individuals who continue to drink alcohol excessively in the presence of liver damage. This underscores the urgent need to address alcohol addiction.
Stop Drinking: Quitting alcohol is the first and most crucial step in overcoming addiction. Seeking professional help, such as through addiction treatment programs, can provide the necessary support for a successful recovery.
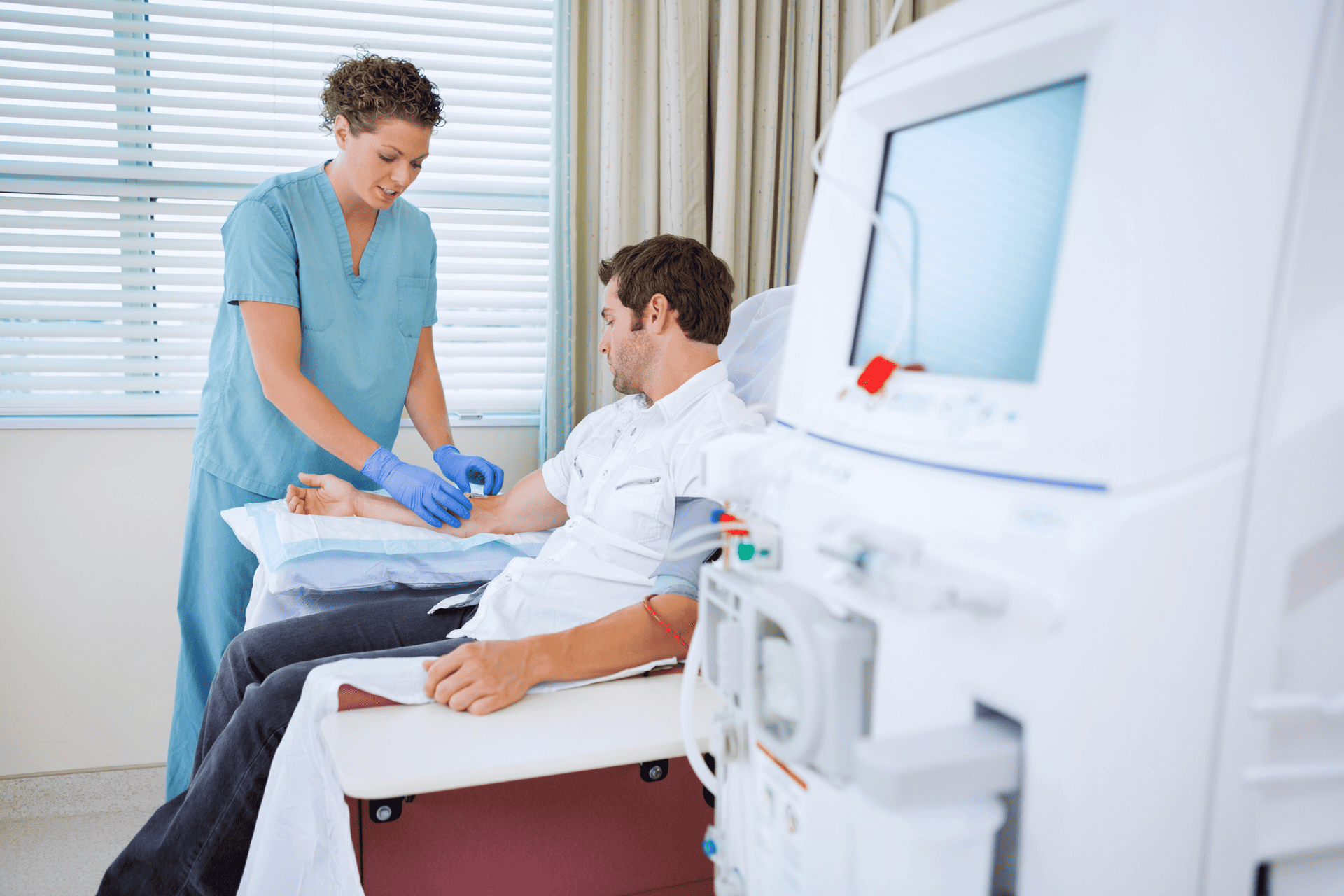
Liver Transplant Units
For individuals with advanced alcoholic liver disease, a liver transplant may be the only option for survival. Understanding the process and considerations for a transplant is essential.
Transplant Evaluation: Individuals with late-stage liver disease are evaluated for liver transplantation. This process includes blood tests and assessing the severity of liver damage and overall health.
Liver Transplant Waitlist: Getting on a transplant waitlist is the next step. The demand for donor livers often exceeds the supply, so wait times can vary.
Post-Transplant Care: After receiving a new liver, individuals require lifelong medical care and medications to prevent rejection and maintain their health.
The liver’s ability to repair itself from heavy drinking also largely depends on the extent of the damage and the individual’s commitment to stop drinking alcohol and make lifestyle changes. While mild cases of alcoholic liver disease may allow for significant recovery, severe conditions like cirrhosis can lead to severe liver disease.
Stop Drinking with the Help of Malibu Detox
At Malibu Detox and Residential Treatment Center, we understand the critical importance of seeking professional help and guidance if you are struggling with alcohol addiction or liver-related issues. Our dedicated team of healthcare providers possesses a wealth of expertise in alcohol-related liver disease, overall health, and addiction treatment. We are committed to delivering personalized advice and unwavering support to individuals facing these complex challenges.
Our integrated approach to treatment is rooted in a deep understanding of the intricate connections between alcohol addiction and liver vitality. We recognize that these issues often intersect and require specialized care. Our team, with a compassionate and empathetic approach, is here to guide you every step of the way.
We pride ourselves on providing a safe and nurturing environment where individuals can embark on their path to recovery. Our comprehensive programs, tailored to your unique needs, encompass detoxification, medical support, therapeutic interventions, and post-treatment planning. We believe in the power of holistic healing, addressing not only the physical aspects of addiction but also the emotional and psychological factors that underpin it. With our unwavering commitment to your well-being, we are here to support you through the journey to a healthier, alcohol-free life and a healthier liver.